Reinventing Healthcare Leadership: Gene Woods’ Journey to Success
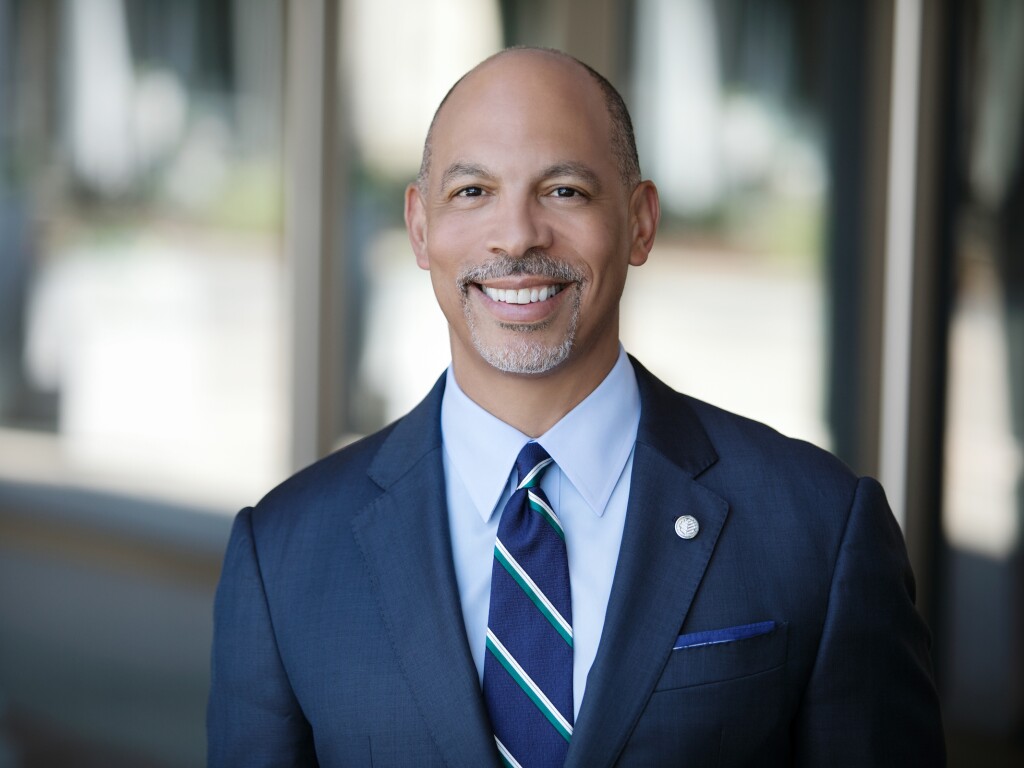
2016 Top 25 Minority Executives in Healthcare–Gene Woods: The best leaders reinvent their organizations, and themselves
2016 Top 25 Minority Executives in Healthcare–Bruce Siegel: Diverse leadership is a must on the road to equity of care

2016 Top 25 Minority Executives in Healthcare–Bruce Siegel: Diverse leadership is a must on the road to equity of care
2016 Top 25 Minority Executives in Healthcare–Patricia Maryland: Taking risks helps leaders grow

2016 Top 25 Minority Executives in Healthcare–Patricia Maryland: Taking risks helps leaders grow
2016 Top 25 Minority Executives in Healthcare–Pamela Sutton-Wallace: Leaders need to challenge themselves to grow

2016 Top 25 Minority Executives in Healthcare–Pamela Sutton-Wallace: Leaders need to challenge themselves to grow
2016 Top 25 Minority Executives in Healthcare: After a complex merger, Ruth Brinkley works to build a new culture at KentuckyOne Health

2016 Top 25 Minority Executives in Healthcare: After a complex merger, Ruth Brinkley works to build a new culture at KentuckyOne Health
Healthcare Leadership: Nicholas Tejeda’s Journey to Success

2016 Top 25 Minority Executives in Healthcare: Nicholas Tejeda responds to healthcare’s need for younger leaders
2016 Top 25 Minority Executives in Healthcare: Wright Lassiter: In healthcare’s new order, no time to bask in past success

2016 Top 25 Minority Executives in Healthcare: Wright Lassiter: In healthcare’s new order, no time to bask in past success
LumiraDx’s Impact: The Sumit Nagpal Story

Top 25 Minority Executives in Healthcare: Sumit Nagpal’s technological innovations at LumiraDx take aim at overhauling care for people with chronic conditions
Medical care is only part of the solution to health disparities

Alameda Health System CEO, Delvecchio Finley, says research shows that access to stable housing, food, education and jobs influences overall health.
Gene Woods’ influential leadership poised to enhance Carolinas HealthCare System
Gene Woods’ influential leadership poised to enhance Carolinas HealthCare System